Pemphigus
Avoiding complex health issues such as allergy need to be identified during the early stages in order to experience the optimum results. Allergens and pollens cause major problems due to which proper health benefits are not realized.
Pemphigus Vulgaris is a severe autoimmune disorder that causes painful blisters and sores on the skin and mucous membranes, primarily in the mouth and throat, and can extend to other areas such as the skin, eyes, and genitals. Early intervention is crucial to manage the disease and prevent complications, including infection, fluid loss, and scarring.
Key Symptoms of Pemphigus Vulgaris:
- Painful Sores and Blisters in the Mouth:
- The initial signs of pemphigus vulgaris often appear as painful sores in the mouth or throat, making it difficult to eat, drink, or swallow.
- Blisters on Skin:
- Blisters on the skin can appear anywhere, often starting in areas like the chest, back, and face. These blisters can rupture easily, leaving painful erosions.
- Oozing and Peeling:
- Blisters are typically filled with fluid, and once they rupture, they leave behind raw, painful skin that oozes and peels.
- Skin Erosions:
- When the blisters rupture, they leave open sores or erosions, which are at high risk for infection if not treated properly.
Effective Treatment Strategies:
- Corticosteroids:
- High-dose corticosteroids (such as prednisone) are the first line of treatment to control inflammation and suppress the immune system. This helps reduce blister formation.
- Immunosuppressive Medications:
- Drugs like azathioprine, mycophenolate mofetil, or methotrexate may be used alongside corticosteroids to help suppress the immune system further and maintain disease control.
- Biologics (Rituximab):
- Rituximab, a monoclonal antibody, is used to target and deplete the specific immune cells that cause pemphigus. It can be particularly effective for people who do not respond to corticosteroids and immunosuppressive drugs.
- Topical Steroids and Immunosuppressive Ointments:
- For mild cases or localized flare-ups, topical steroids and immunosuppressive treatments can help reduce inflammation and prevent new blisters from forming.
- Wound Care:
- Since pemphigus vulgaris causes painful, open sores, careful wound management is essential to prevent infection. Regular cleaning and dressing of affected areas are important.
- Pain Management:
- Due to the painful nature of the condition, pain management, including analgesics and topical numbing agents, may be prescribed to provide relief.
- Antibiotics:
- To prevent or treat secondary infections caused by open sores, antibiotics may be necessary.
Importance of Timely Intervention:
- Prevention of Complications: Early treatment is key to controlling symptoms and preventing infections, scarring, and long-term damage.
- Quality of Life: Managing pain and discomfort effectively improves overall well-being, allowing patients to maintain a better quality of life.
- Long-Term Monitoring: Pemphigus vulgaris is a chronic condition, requiring ongoing monitoring and treatment adjustments to maintain remission and prevent flare-ups.
Consulting with a dermatologist or an autoimmune disease specialist is essential to determine the most effective treatment plan based on the severity and progression of the disease.
Advanced treatment for pemphigus vulgaris is vital to ensure effective management of the condition, reduce flare-ups, and prevent long-term complications such as infections, scarring, and organ damage. Working closely with experienced healthcare professionals is crucial for determining the best treatment strategy tailored to each patient’s needs. Below are some advanced treatment options and additional solutions to manage pemphigus vulgaris effectively.
Corticosteroid Treatment:
Corticosteroids (e.g., prednisone) are the cornerstone of pemphigus vulgaris treatment. While effective in reducing inflammation and controlling blistering, long-term use can lead to side effects like cataracts, glaucoma, and other complications. To mitigate these risks, doctors may monitor the patient’s eye health and adjust the dosage over time.
Managing Side Effects:
- Cataracts and glaucoma are potential risks of prolonged corticosteroid use. Regular eye exams are crucial to detect and address these conditions early.
- Bone health may be impacted, so calcium and vitamin D supplements are often prescribed to help prevent osteoporosis.
Additional Treatment Options:
- Vitamin D Supplements:
- Vitamin D plays a critical role in immune function and skin health. For patients on corticosteroid treatment, which can interfere with calcium absorption, supplementing with Vitamin D can help maintain bone density and overall health.
- Vitamin D also supports the immune system, which is essential for managing autoimmune disorders like pemphigus vulgaris.
- Plasmapheresis:
- Plasmapheresis, also known as therapeutic plasma exchange, is an advanced procedure that removes antibodies from the blood that attack the skin. This treatment is especially beneficial for severe or refractory cases of pemphigus vulgaris where standard therapies have failed.
- It helps to reduce the level of autoantibodies in the blood, improving symptoms and hastening the healing process.
- Plasmapheresis is typically used in combination with other treatments, such as corticosteroids and immunosuppressive drugs, for optimal results.
Other Treatment Solutions:
- Immunosuppressive Drugs:
- Medications such as azathioprine, mycophenolate mofetil, or methotrexate can be used to reduce the need for corticosteroids and help manage the immune response. These drugs work by suppressing the overactive immune system that causes the blisters and sores.
- Biologic Therapy:
- Rituximab is a biologic drug that targets specific immune cells responsible for the formation of antibodies in pemphigus vulgaris. It is often used in cases where corticosteroids and immunosuppressive drugs are insufficient.
- Wound Care:
- Proper wound management is essential, as the blisters can lead to painful, open sores. Regular cleaning, dressing, and possible use of topical antibiotics can prevent secondary infections and promote faster healing.
Consulting an Experienced Specialist:
- Timely Diagnosis: Recognizing the early signs of pemphigus vulgaris, such as painful mouth blisters and skin erosions, is essential for early intervention.
- Long-term Management: Pemphigus vulgaris is a chronic condition, and regular check-ups with a dermatologist or immunologist will help monitor disease progression and adjust treatment accordingly.
Conclusion:
Pemphigus vulgaris is a serious condition that requires timely and comprehensive care to avoid complications. Advanced treatments such as plasmapheresis, corticosteroid management, and vitamin supplementation help control the disease, improve quality of life, and reduce side effects. Consulting with experienced specialists and tailoring the treatment plan to the patient's needs is key to achieving the best outcomes.
Pemphigus vulgaris, along with other autoimmune diseases, can have significant effects on the body, which is why early identification and treatment are crucial to minimizing complications and ensuring the best possible health outcomes. Understanding the disease's causes and effects will help individuals take proactive steps in managing their health and avoiding further issues.
Effects of Pemphigus Vulgaris:
- Stomach Ulcers:
- People with pemphigus vulgaris may experience gastrointestinal issues, including stomach ulcers. The condition's autoimmune nature can sometimes lead to inflammation of the stomach lining, which may develop into ulcers. Corticosteroid treatments used to manage pemphigus can also contribute to gastrointestinal distress, as they can irritate the stomach lining.
- Extreme Loss of Muscle Mass:
- Muscle wasting (atrophy) can occur in people with pemphigus vulgaris due to prolonged corticosteroid treatment. Corticosteroids, while essential for managing the disease, can lead to muscle weakness and loss of muscle mass when used for long periods. This side effect can be mitigated with physical therapy, protein supplements, and other strategies to help maintain muscle strength.
- Painful Mucous Membrane Damage:
- Pemphigus vulgaris often affects the mucous membranes, particularly the mouth, throat, and genitals. The blistering and erosions can cause severe pain and difficulty swallowing or speaking. The oral lesions may also make it challenging to maintain proper nutrition and oral hygiene.
Causes of Pemphigus Vulgaris:
- Weakening of the Immune System:
- Pemphigus vulgaris is an autoimmune disease, meaning the body's immune system mistakenly attacks its own healthy cells. The immune system produces antibodies that target specific proteins in the skin and mucous membranes, leading to the development of blisters and erosions. This process weakens the skin's structural integrity, making it prone to damage.
- Severe Effects on Mucous Membranes:
- Pemphigus vulgaris primarily affects the desmosomes (the structures that hold skin cells together), which causes the skin to break apart, forming blisters. The disease often starts with blisters in the mouth and mucous membranes, where it can be most painful and difficult to treat.
How long does it take to have a pigmentation treatment?
Treatment might range from 5 to 30 minutes, depending on the area of the treatment. Need of topical anaesthetic should be discussed with doctors beforehand. How many pigmentation treatments are required? Most patients may notice considerable improvement after 1 to 4 treatments, varying based on the skin condition and treatment intensity.
How long do the effects last?
Results can reduce signs of ageing and pigmentation, but treatments won't pause the process. Follow-up treatments and a daily sunscreen practice can help you get consistent results.
What is Pemphigus?
Pemphigus is a rare autoimmune condition that causes skin blisters and mucous membranes. It happens when the immune system mistakenly targets healthy cells, resulting in painful blisters.
How to manage Pemphigus symptoms and after treatment?
Managing Pemphigus symptoms requires appropriate skincare practices, avoiding triggers, and maintaining general health. Even after successful treatment, it is advised to have regular check-ups with a healthcare expert to detect and address any signs of recurrence.
What is the normal duration of Pemphigus treatment?
Treatment duration varies from person to person. Some people may only need treatment for a short time, while others may require continuous treatment to regulate their symptoms.
Is it possible for Pemphigus to worsen?
Yes, problems such as secondary infections, sepsis, and fluid imbalance can occur as a result of pemphigus. To avoid problems, timely and appropriate treatment is essential.
What is the treatment for Pemphigus?
Systemic corticosteroids are commonly prescribed to suppress the immune system during treatment. Immunosuppressive medications and, in certain situations, intravenous immunoglobulin (IVIG) or plasmapheresis may be prescribed.
Is Pemphigus a hereditary disease?
While there is a hereditary genetic vulnerability, pemphigus is not inherited directly. It is mostly an autoimmune condition.
What is the cause of Pemphigus?
Pemphigus is caused by the immune system mistakenly attacking proteins necessary for the normal functioning of the skin and mucous membranes.
How is Pemphigus identified?
A skin biopsy, blood tests, and an examination of clinical symptoms are usually used to make a diagnosis. To establish the existence of antibodies, immunofluorescence tests are often done.
What are the Pemphigus symptoms?
Painful Blisters on the skin and mucous membranes which may tear quickly, creating open wounds. Severe cases might cause major blistering.
Is Pemphigus infectious?
Pemphigus does not spread. It is an autoimmune condition that cannot be passed on through contact with an affected person.
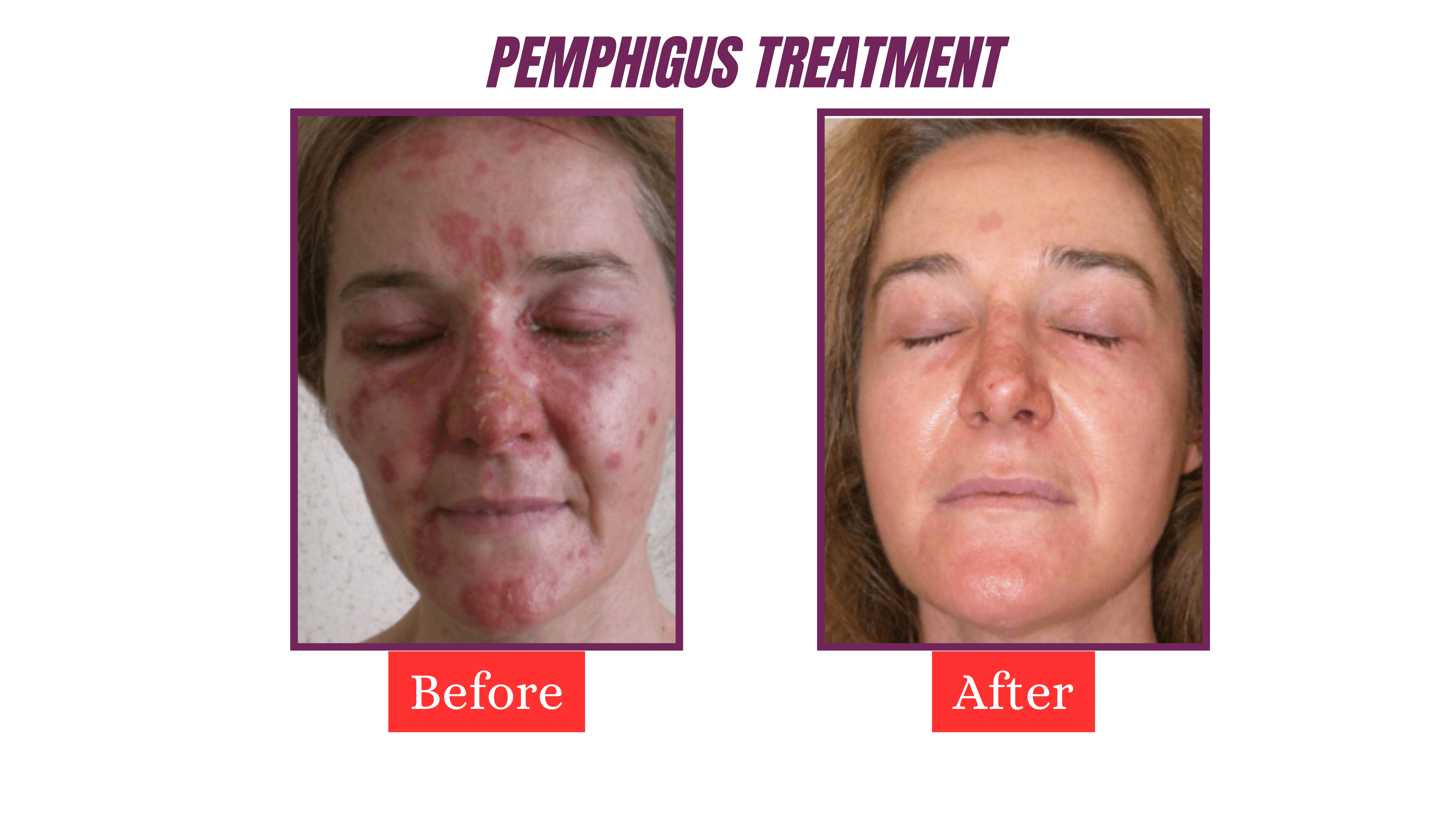
Results